Types of Depression—Exploring the Spectrum
Uncover the diverse faces of depression in our guide. From major to seasonal, explore the types of depression and their unique signs for better understanding and support.
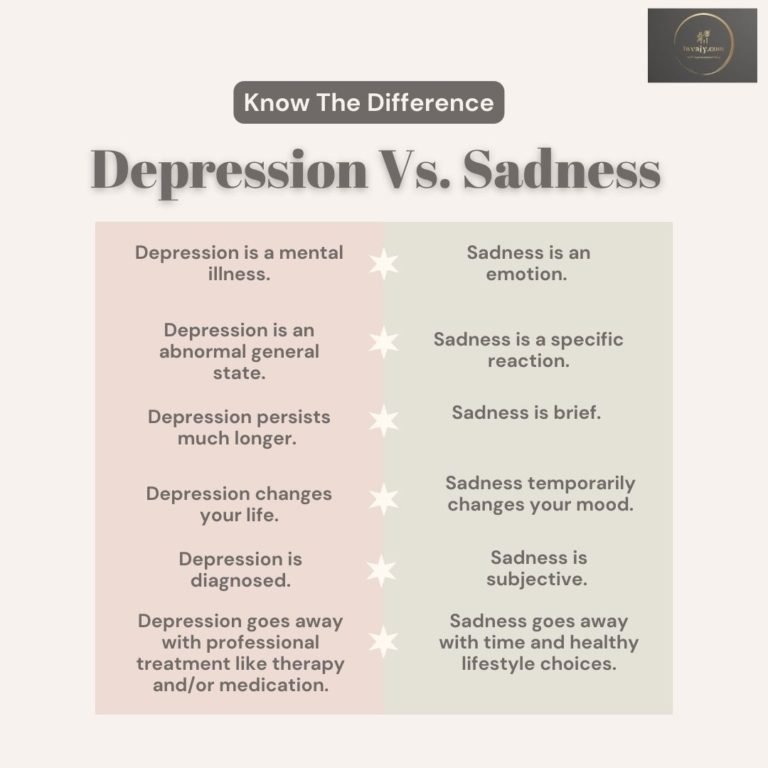
Depression goes beyond just feeling sad. Everybody feels low, upset, frustrated or unmotivated from time to time. Depression is much more complicated than simply being “down in the dumps”. Depressive disorder is a mood disorder. It affects how a person thinks, feels, and behaves. Signs and symptoms of depression can range dramatically, from hopelessness and fatigue to a loss of interest in life, physical pain, and suicidal thoughts.
Depression, a multifaceted mental health condition, is far from a monolithic experience. Depression can be thought of as an umbrella term for a variety of disorders. The term encompasses a spectrum of disorders, each distinguished by unique characteristics, symptoms, and underlying factors. Some of these disorders are caused by certain life events or situations, and others by chemical changes in the brain. What’s more, while some of the symptoms associated with the various depressive disorders overlap, there are also some key differences. This article aims to provide an in-depth exploration of different types of depression, shedding light on the diverse nature of this pervasive mental health challenge.
Major Depressive Disorder – MDD (Clinical Depression)
The Common Denominator
Major Depressive Disorder, often referred to as unipolar depression or clinical depression, stands as the primary archetype of depression. Characterized by persistent feelings of sadness, hopelessness, feelings of worthlessness or guilt and a profound lack of interest or pleasure in daily activities, MDD affects millions worldwide. To meet the diagnostic criteria, these symptoms must persist for at least two weeks, significantly impairing one’s ability to function.
MDD is more than just a collection of symptoms; it’s a pervasive cloud that obscures the vibrancy of life. From the outside, it might be challenging to grasp the depth of despair that individuals with MDD experience. This type of depression is often accompanied by physical symptoms, such as changes in appetite and sleep patterns, fatigue, weight loss/gain and difficulty concentrating.
People suffering from Clinical Depression feels restless or agitated, have irritability and sometimes experience suicidal thoughts.
Persistent Depressive Disorder – PDD (Dysthymia)
The Chronic Shadow
Formerly known as dysthymia, Persistent Depressive Disorder extends its reach beyond the acute phases of MDD. Individuals grappling with PDD experience a milder, yet chronic form of depression that lasts for two years or more. The longevity of symptoms distinguishes PDD, making it a persistent shadow cast over an individual’s life.
PDD might not deliver the acute blows of MDD, but its chronic nature can be equally debilitating. The persistent low mood and feelings of inadequacy become integral aspects of one’s identity, impacting various spheres of life, including work, relationships, and personal pursuits.
People with dysthymia often find it difficult to be happy even on typically joyous occasions. People around them might perceive them as gloomy, pessimistic, or as a complainer. However, in reality, they are dealing with a chronic mental illness.
Manic Depression (Bipolar Disorder)
Riding the Emotional Rollercoaster
Bipolar Disorder introduces a unique twist to the narrative of depression. This mood disorder is characterized by extreme mood swings, oscillating between depressive episodes and manic or hypomanic states. The depressive phase shares similarities with MDD, but the hallmark of bipolar disorder is the unpredictable shift to elevated, often euphoric, moods.
The pendulum swings of bipolar disorder can be emotionally exhausting. Individuals may find themselves caught between the depths of despair and the exhilaration of mania, struggling to maintain stability. Recognizing the cyclical nature of this disorder is crucial for accurate diagnosis and effective management.

In the clinical setting, bipolar comes in several forms, including bipolar 1 and bipolar 2. All types of bipolar disorder involve extreme highs and lows. The main difference between bipolar 1 and bipolar 2 is the severity of the manic symptoms. With bipolar 1 the mania is typically more severe. With bipolar 2, the individual experiences hypomania, a less severe form of mania that results in behaviors that are atypical for the individual but not abnormal to society at large.
Seasonal Affective Disorder (SAD)
When Seasons Shape Emotions
Seasonal Affective Disorder, or SAD, manifests as recurrent depressive episodes tied to specific seasons, most commonly winter. Linked to reduced exposure to natural sunlight, SAD underscores the intricate interplay between environmental factors and mental health.
The changing seasons may bring joy to some, but for those with SAD, the onset of winter signals a descent into a mental and emotional abyss. Those who experience SAD in the winter have also have unique symptoms – heaviness in arms and legs, frequent oversleeping, cravings for carbohydrates/weight gain and relationship problems.
Light therapy, increased exposure to natural light, and lifestyle adjustments can be integral components of the treatment plan for SAD.
Psychotic Depression
A Twist of Reality
Psychotic Depression adds a layer of complexity to the depressive experience by introducing psychotic features. Individuals with this type of depression may experience delusions or hallucinations, amplifying the distress associated with the disorder.
Psychotic depression blurs the lines between reality and imagination. It demands careful assessment and a comprehensive treatment approach that addresses both the depressive symptoms and the psychotic features.
According to the National Alliance on Mental Illness, around 20 percent of people with depression have episodes so severe that they develop psychotic symptoms.
Atypical Depression
Defying the Norms
Despite its name, atypical depression may in fact be one of the most prominent types of depression. Atypical depression is different from the persistent sadness or hopelessness that characterizes major depression. It is considered to be a “specifier” or subtype of major depression that describes a pattern of depression symptoms, including – oversleeping, overeating, irritability, heaviness in the arms and legs, sensitivity to rejection, and relationship problems. One of the main hallmarks of atypical depression in the ability for the mood of the depressed individual to improve following a positive event.
Atypical Depression challenges the stereotypical image of depression. Atypical depression presents a paradox, with symptoms that may initially seem counterintuitive to the typical signs of depression.
Just like any type of depression, atypical depression is a serious mental health condition. Patients with this type of depression have an increased risk of suicide and anxiety disorders. Atypical depression often starts in the teenage years, earlier than other types of depression, and can have a more long-term (chronic) course.
Recognizing these atypical features is crucial for accurate diagnosis and targeted treatment.
Postpartum Depression (Peripartum Depression)
Navigating Motherhood's Shadows
Motherhood is often romanticized, but for some, it brings about a significant mental health challenge. PPD highlights the profound impact hormonal changes, sleep deprivation, and the stresses of new parenthood can have on mental well-being.
Sad feelings and crying bouts that follow childbirth are known as the “baby blues.” The baby blues are common and tend to decrease within a week or two. Around one in seven women will experience something more extreme than the typical baby blues. Women that give birth and struggle with sadness, anxiety or worry for several weeks or more may have postpartum depression (PPD). Sometimes it’s called peripartum depression because it can start during pregnancy and continue after childbirth.

The joy of bringing a new life into the world can be overshadowed by the dark clouds of postpartum depression. This type of depression requires sensitive and comprehensive support, recognizing the unique challenges faced by new mothers.
Premenstrual Dysphoric Disorder (PMDD)
The Monthly Struggle
Premenstrual Dysphoric Disorder or PMDD is a severe form of premenstrual syndrome (PMS), affecting some women in the days leading up to menstruation. Emotional symptoms, including irritability, sadness, and mood swings, are more pronounced than those typically associated with PMS. That said, behavioral and physical symptoms also occur.
PMDD underscores the intricate interplay between hormonal fluctuations and mood. Recognizing the cyclic nature of PMDD symptoms is essential for effective management and support.
While up to 85% of women experience PMS, only around 5% of women receive a diagnosis of PMDD.
Situational Depression (Reactive Depression/Adjustment Disorder)
When Life Takes a Toll
Situational Depression, also known as as reactive depression or adjustment disorder, is a reactive form of depression triggered by specific events or life circumstances. While the symptoms may be temporary, they can be severe and impact various aspects of daily life.
Situational Depression can develop after a person experiences a traumatic event or a series of changes to their everyday life. Examples of events or changes that may trigger situational depression include but are not limited to: divorce, retirement, loss of a friend, illness, loss of job, and relationship problems.
The ebb and flow of life events can take a toll on mental health. Situational depression demands a nuanced approach that addresses both the underlying stressors and the emotional toll they take.
Most people who experience situational depression begin to have symptoms within about 90 days following the triggering event.
Double Depression
The Intersection of PDD and MDD
Double Depression represents a challenging convergence of Persistent Depressive Disorder (PDD) and Major Depressive Disorder (MDD). Individuals with double depression endure chronic low-grade depressive symptoms (PDD) punctuated by intermittent episodes of more severe depression (MDD), creating a layered and intricate clinical picture.
Double depression is a diagnostic challenge, requiring a careful examination of symptom patterns over time. Treatment approaches need to address both the persistent nature of PDD and the acute exacerbations of MDD.
Disruptive Mood Dysregulation Disorder (DMDD)
The Childhood Disruptor
Disruptive Mood Dysregulation Disorder (DMDD) is a fairly recent diagnosis, appearing for the first time in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. The DSM-5 classifies DMDD as a type of depressive disorder, as children and and adolescents diagnosed with DMDD struggle to regulate their moods and emotions in an age-appropriate way. As a result, children with DMDD exhibit frequent temper outbursts in response to frustration, either verbally or behaviorally. In between outbursts, they experience chronic, persistent irritability.
Wrapping Up!—
This comprehensive exploration of types of depression underscores the intricate and multifaceted nature of this mental health challenge. Recognizing the diversity within the spectrum of clinical depression is paramount for accurate diagnosis and effective treatment. Mental health professionals, armed with a nuanced understanding of these variations, can tailor interventions to address the unique needs of individuals grappling with different forms of depression. By fostering awareness and understanding, we take a significant step towards destigmatizing depression and promoting a more empathetic and informed approach to mental health. If you or someone you know is experiencing symptoms of depression, seeking professional help is crucial for a comprehensive assessment and the development of a personalized path to recovery.